HURLBURT FIELD, Fla. -- An elite team of Air Force medical professionals who forward-deploy to austere environments is pushing the standard of care while in the field.
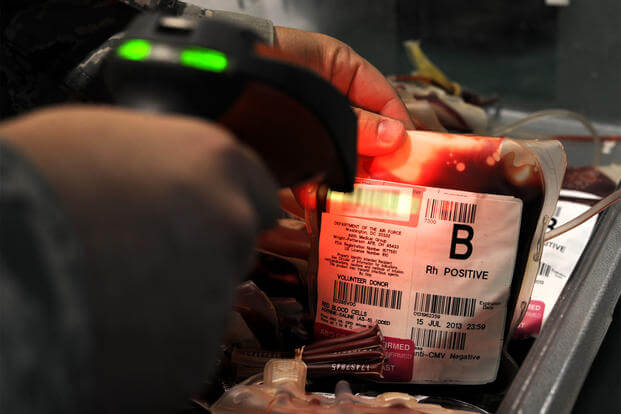
"Blood supply and resupply was the biggest challenge. It's a challenge we were fighting everyday," said Maj. Marc Northern, a surgeon with the 720th Operations Support Squadron here. Northern is part of a six-member Special Operations Surgical Team that deployed to the Middle East during Operation Inherent Resolve between April and September 2017.
Military.com caught up with the team last month on a trip accompanying Air Force Secretary Heather Wilson to the base.
During the deployment, U.S. soldiers would come in and sit for hours donating blood. Blood donation banks worked round the clock. And members of the team found themselves donating, too.
Related content:
- 4 Airmen to Receive Bronze Star for Saving Lives in ISIS Fight
- Future of Combat Medicine: Powdered Blood, Spray Bottle Skin
- Air Force to Double Number of Combat Aviation Advisors
A blood warmer would help, the team members said. It's a solution the AFSOC teams hope they can soon procure for their makeshift trauma rooms.
Without disclosing what kind of warmers they use now, members said it takes time to generate enough heat to get the frozen blood packs fluid -- time most patients don't have.
"Sometimes, we stick the blood packs in our armpits [and massage them] to get the blood going," said Maj. Dan Farber, an anesthesiologist.
"Cold kills our patients," said Maj. Kristopher Filak, an emergency room doctor and the team lead. "Keeping them warm and keeping them from hypothermia is key."
Freeze-dried plasma may also help fill a gap, Northern said. The method, which dates back to World War II, is more stable and portable than frozen plasma. All units have to do is add sterile water and inject. But the technique has not been approved by the Food and Drug Administration, Northern said. Some units have used it in testing scenarios. This particular team did not use freeze-dried plasma in the field.
The team said they need a device small enough to transport and efficient at warming blood packs quickly to transfuse into a patient, after taking the blood out of cold storage.
Air Force Special Operations Command has a medical modernization unit that help the teams search for the "latest and greatest, lightest, battery-operated equipment," Northern said.
"It's got to be battery-operated, durable, and [has to] be able to fuse it in the right amount of time, and those are all very strict requirements we've given to … medical modernization who then in turn work with civilian companies to develop a product," Filak said.
For example, AFSOC recently replaced an ultrasound machine that looked like a portable, flip Gameboy player. Teams estimate technologies like this become outdated in five to six years, so they work with medical modernization to keep equipment as up-to-date as possible.
SOSTs deployed right now are using a new, updated ultrasound machine, but while Northern said updated tech is helpful, it's the people who make the team work.
"We have to be intuitive or progressive with how you're thinking," Faber added, especially given the number of people the teams help save.
During their deployment, "our team had the largest surge" of patients, said Maj. Regan Lyon, an emergency medical physician with the 720th.
In February, a team of five received Bronze Stars for their work in Syria in 2016. That team treated more than 750 patients, in some cases under direct assault by Islamic State fighters.
While Lyon and Northern's team didn't experience enemy fire, in 120 days they treated 1,011 patients, some with blast or gunshot wounds. Their patients were mostly civilians, including children, as well as three military working dogs, AFSOC said.
The team achieved a 90 percent patient survival rate -- if they came in alive, they likely left alive, Northern said.
"We're always pushing for taking the best technologies from the U.S. standard and pushing that as far forward as we can," he said.
This mission "varies," said Filak. "We fill that gap between the first injury and a hospital room. We go wherever they need us."
-- Oriana Pawlyk can be reached at oriana.pawlyk@military.com. Follow her on Twitter at @Oriana0214.