The Defense Department has acknowledged systemic problems in the vast Military Health System (MHS) for active-duty and retired troops similar to the pattern of poor care and management that has plagued the Department of Veterans Affairs.
"The people we serve expect us to improve. The American public expects us to improve. We expect ourselves to improve," Dr. Jonathan Woodson, the assistant secretary of Defense for Health Affairs, said in a recent memo to all medical personnel.
Woodson sent the memo following New York Times reports based on months of investigation showing "a pattern of avoidable errors that has led to injuries and contributed to some deaths" in MHS facilities.
The reports documented widespread problems in infection control and patient safety, and found that babies born in military hospitals were twice as likely to suffer injuries as newborns nationally.
Mothers giving birth at MHS facilities also were significantly more likely to hemorrhage after childbirth than mothers at civilian hospitals, the reports said.
Pentagon officials did not dispute the Times' reports. The reports instead were seen as a guideline to help "determine exactly where we are" in reforming the system, said Army Col. Steve Warren, a Pentagon spokesman.
The MHS has 56 hospitals and 361 clinics worldwide serving "9.6 million beneficiaries" in a system that is separate from the VA. The beneficiaries include 1.45 million active-duty service members, 1.7 million active-duty family members and 610,000 retired service members.
The beneficiaries are served by more than 133,000 military and civilian doctors, nurses, medical educators, researchers and other health professionals.
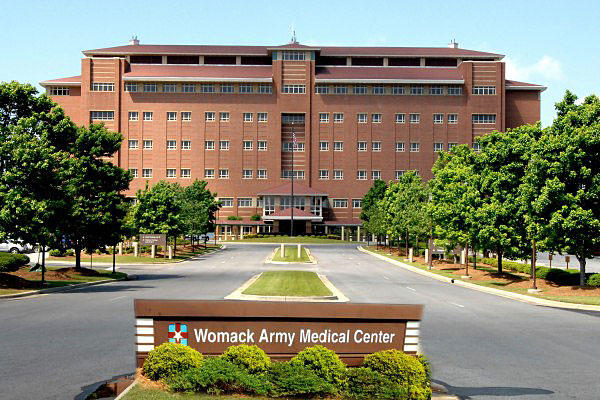
The first public signs of a crisis came in May with the firing of Col. Steven Brewster, commander of the Womack Army Medical Center at Fort Bragg, N.C. Brewster was relieved after Lt. Gen. Patricia Horoho, the Army's Surgeon General, and other superiors "lost trust and confidence" in him.
Horoho, the former head nurse at Womack, also suspended the deputy commanders for clinical services, nursing and administration at Womack.
Earlier this year, Womack officials had delayed medical procedures over concerns with the accreditation of the hospital that serves the largest population of medical beneficiaries in the Army.
The New York Times reported that Brewster's ouster was partly related to the death of Racheal Marie Rice, a 29-year-old wife of a Fort Bragg soldier and mother of three, who died the morning after a routine procedure at Womack.
A Fort Bragg release said that Brewster was relieved "to address the changes needed to maintain a high level of patient care. Investigations into these issues are ongoing, and further action will be forthcoming."
Shortly after Brewster's firing, Rep. Renee Ellmers, R-S.C., whose district includes Fort Bragg, issued a statement saying "reports of substandard care for our country's warriors and veterans sent shock waves throughout the Fort Bragg community."
Following a meeting with Col. Ronald Stephens, the acting director at Womack, Ellmers said Fort Bragg and Army leaders "assured me that the ongoing investigation will be dealt with in a way that holds people accountable."
The day after Brewster was relieved on May 26, Hagel ordered a 90-day review of MHS. Hagel gave the job of overseeing the worldwide review to new Deputy Defense Secretary Robert Work, a retired Marine colonel and former executive of a Washington think tank.
Rear Adm. John Kirby, the Pentagon press secretary, said the review was being undertaken with the scandal over waiting lists and poor treatment at VA facilities in mind.
"It's clearly within the context of what he [Hagel] is watching at the VA," Kirby said. "He wants to know what we don't know. He doesn't want to wait for similar allegations to appear with the active military healthcare system."
The review was to include town hall meetings for staff and patients at San Diego Naval Hospital; Madigan Army Hospital at Joint Base Lewis-McChord; Winn Army Hospital at Fort Stewart; Lakenheath Air Force Hospital in Britain; Fort Belvoir Community Hospital in Virginia; the Air Force Academy Cadet Clinic; and the Patuxent River Naval Clinic in Maryland.
Hagel has also directed Work to solicit the advice of outside experts on reforming MHS. Work's report is due to Hagel on Aug. 29.
The need for changes in the way the MHS operates comes at a time when Hagel and the service chiefs have been seeking to cut or at least slow the growth of health care costs in the military. In testimony to Congress, Hagel has repeatedly pointed out that military health care costs have more than doubled since 2001 to the current annual cost of about $52 billion.
The White House Office of Management and Budget (OMB) projected that slowing the growth of Tricare costs for military retirees would result in savings of $902 million in Fiscal 2014 and $9.3 billion through FY 2018. Those savings were needed to offset projected increases in personnel and readiness costs, OMB said.
The problems in care and management at the MHS have also come at a time when MHS has been undertaking a major shift in the way it delivers services.
In a March message from MHS leadership to employees, MHS said that "after more than a decade of war and in a period of national evolution in concepts of health care, the Military Health System must re-engineer processes by which we bring health to the 9.6 million beneficiaries we serve."
The message said that the focus would shift to a "patient-centered medical home model," which was described as being "central to our strategy to form a partnership with each patient for whom we provide primary care."
The home model "holds promise as a way to improve health care in America by transforming how primary care is organized and delivered," MHS said.
The intent was to provide "primary health care that is relationship-based with an orientation toward the whole person. Partnering with patients and their families requires understanding and respecting each patient's unique needs, culture, values and preferences," MHS said.
-- Richard Sisk can be reached at Richard.Sisk@monster.com.