FORT DETRICK, Md. -- The tongue is an amazing organ.
Thousands of nerve fibers in it help us eat, drink and swallow. Without them, we would not taste. The tongue helps us speak. Quietly, its surface defends our bodies from germs.
Yet for everything the tongue can do, perhaps one of its most exciting roles is to serve as a direct "gateway" to the brain through thousands of nerve endings.
Now researchers at the U.S. Army Medical Research and Materiel Command in collaboration with the University of Wisconsin-Madison and NeuroHabilitation Corporation are leveraging the power of those tiny nerves. They are aiming to restore lost physical and mental function for service members and civilians who suffered traumatic brain injury or stroke, or who have Parkinson's or multiple sclerosis.
The treatment involves sending specially-patterned nerve impulses to a patient's brain through an electrode-covered oral device called a "PoNS," a battery-operated appliance placed on the tongue. The 20-30 minute stimulation therapy, called cranial nerve non-invasive neuromodulation, or CN-NiNM, is accompanied with a custom set of physical, occupational, and cognitive exercises, based on the patient's deficits. The idea is to improve the brain's organizational ability and allow the patient to regain neural control.
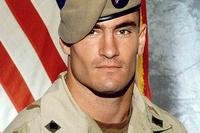
NeuroHabilitation Corporation is funding the commercial development of the device, and has more than just financial investments in PoNS. The company was created with support by Montel Williams, a celebrity and military veteran who was diagnosed with multiple sclerosis in 1999.
Williams was originally introduced to the research through an American Way magazine an attendant gave to him while he was on an American Airlines flight. The magazine included an article about work being done at the University of Wisconsin-Madison. Shortly after reading the article, Williams joined a study at the University of Wisconsin-Madison's Tactile Communication & Neurorehabilitation Lab, which is in the Department of Biomedical Engineering.
"The third day there I said we need this in the mouths of our Soldiers," recalled Williams, stating that he has always kept his ties with the military after serving in the Marine Corps and graduating from the U.S. Naval Academy.
The PoNS prototype and associated therapeutic use were developed by University of Wisconsin-Madison scientists Yuri Danilov, Ph.D., Mitchell Tyler, M.S., P.E., and Kurt Kaczmarek, Ph.D. Their research is driven by the principle that brain function is not hardwired or fixed, but can be reorganized in response to new experiences, sensory input and functional demands. This area of research is called neuroplasticity and is a promising and rapidly growing area of brain research.
Preliminary data from University of Wisconsin showed CN-NiNM to have great potential for a wide variety of neurological issues. Remarkably, the therapy doesn't only slow functional loss, but also has the potential to restore lost function. That's why researchers are saying that it "breaks the rules."
"When we talk about a brain changing itself, this is what we mean," said Danilov.
Because of its possible application for service members, especially those returning from combat with blast-related traumatic brain injuries, the USAMRMC signed a Cooperative Research and Development Agreement with NeuroHabilitation Corporation (founded by Williams and his colleagues, including the University of Wisconsin scientists), Feb. 8, that allows the Army to further evaluate the device.
"This exciting agreement leverages a unique private-public partnership," said Col. Dallas Hack, director of the USAMRMC Combat Casualty Care Research Program. "By collaborating with University of Wisconsin-Madison and NeuroHabilitation Corporation, we maximize our resources to explore a potential real-world treatment for injured service members and civilians with a variety of health conditions."
Testing will include a collaborative study with researchers and clinicians at the Blanchfield Army Community Hospital in Fort Campbell, Ky., due to start this month as the result of a year-long coordination effort led by Capt. Ian Dews, deputy director of CCCRP. The hospital is home to the Warrior Resiliency and Recovery Center, which is dedicated to the treatment of Soldiers with physical and neuropsychological problems due to service-related trauma.
Additional patient testing will be conducted at other Veteran facilities and civilian medical institutions. Concurrently, the USAMRMC, in collaboration with its subcommands the U.S. Army Medical Materiel Agency and the U.S. Army Medical Materiel Development Activity, will conduct environmental testing, such as temperature and humidity limitations for the device, to better understand potential constraints. At the conclusion, the USAMRMC hopes to seek U.S. Food and Drug Administration clearance for PoNS.